At Cassie + Friends, we believe that every child and family should have access to timely and optimal rheumatic disease care. That’s why we launched the C+F Northern BC Project, to better understand the barriers to diagnosis, care, and patient support for families living in remote/rural communities and explore how we can work together to improve support. You can read more about what we found here.
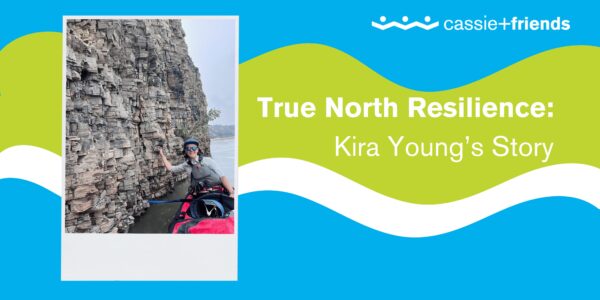
At the core of our learning sits lived experiences and stories that highlight the diversity of rheumatic disease experiences across Canada, including Kira Young’s, a youth navigating an autoinflammatory disease diagnosis who has shown true North resilience in her pursuit of equitable access to healthcare. Here is her story.
Hello! My name is Kira, and I am from Yellowknife, Northwest Territories. I’m currently 18 years old and just finished high school this past June. In September 2024, I began an Arts and Science Degree program at McMaster University.
A cornerstone of my experience with rheumatic disease is where I live. I grew up paddling and cross-country skiing on the lakes and rivers around Yellowknife and I have more recently come to appreciate its robust community and unique location. Up until my illness began in 2022 the relative isolation of Yellowknife was never a big problem, but I quickly became familiar with a challenge that many people across Canada face, especially in the North: displaced healthcare.
It took nearly 2 years to get an accurate diagnosis after initially getting sick – and even with that, my “disease” hasn’t actually been given a name: it is classified as “autoinflammatory disease, not otherwise specified”, but is very similar to sJIA in kids and Still’s Disease in adults (that’s how my doctors refer to it).
In the Northwest Territories, there are no rheumatologists and there is very little capacity for critical illness. I have been medevaced to Edmonton 6 times, a journey that is long and riddled with logistical and bureaucratic challenges that are familiar to anyone who has to travel to see their doctor. For example, health information does not flow easily across provincial and territorial borders. When in Alberta, my doctors could not access my NWT health records, and vice versa, unless my healthcare team went to extraordinary lengths (using outdated technology – fax) to send information back and forth, often with a significant delay.
In the Fall of 2023, I was medevaced to Edmonton twice due to a complication of my disease, called Macrophage Activation Syndrome (which can accompany Juvenile Arthritis in some cases). I spent close to 2 weeks in the intensive care unit, where I lost my hair and a lot of my muscle mass, and then spent many more weeks recovering in Edmonton, over a thousand kilometres from my family, my friends, and my home.
Now that I am on a treatment that keeps my disease under control and has allowed me to return to school, to running, playing the guitar, and to everything else I love to do, I routinely see my rheumatologist virtually or I travel to Edmonton. A silver lining of this undeniably difficult situation is that I have gained a lot of insight into an experience that is not uncommon in Canada, especially for people living with rare and/or rheumatologic diseases. Displaced healthcare in any capacity, but especially inter-provincially or territorially, presents a very unique set of challenges to young people and their families.
Travelling for healthcare and being sick away from home is uniquely difficult and can be isolating, it’s easy to feel alone in this experience. That’s one of the reasons I connected to Cassie + Friends and felt that it was important to share my story with others. I recognize and empathize with the unique challenges that come with being far removed from healthcare and hope that by using our collective voices to raise awareness of these inequities we can do better for kids and families across Canada.






Leave A Comment