nutrition + rheumatic disease
What is the role of nutrition in swelling, pain and stiffness in JA and other rheumatic diseases?
From the SickKids News Rheum, Issue Fall 2020: Nutrition Edition
What we eat is very important for our health and wellbeing. The same is true for people with rheumatic conditions. Rheumatic conditions are a group of diseases that can make joints, tendons, ligaments, bones or muscles inflamed. This means that these areas become red, swollen, warm to the touch, stiff and painful. Rheumatic conditions are diseases like juvenile arthritis (JIA), rheumatoid arthritis, psoriatic arthritis, systemic lupus erythematosus, ankylosing spondylitis, dermatomyositis and others.
There are no cures for rheumatic conditions but taking medication can help reduce pain and swelling. Many people with rheumatic conditions are also interested to learn if there are other ways to help with pain and swelling, like nutrition. While some studies suggest that avoiding meat, animal products or gluten may help with swelling or pain, at this time there is no diet that can treat or cure a rheumatic condition. Studies do however tell us that nutrition plays an important role in helping to manage health.
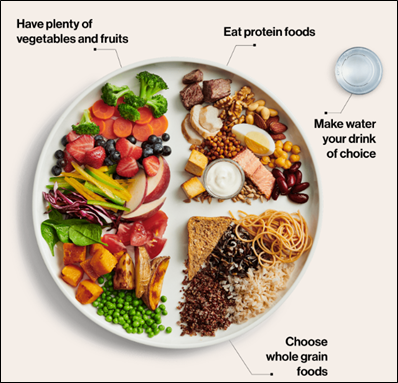
Many Canadians and people with rheumatic conditions are encouraged to eat a healthy diet. For example, research shows that eating a Mediterranean diet can help reduce pain, swelling and stiffness in people with rheumatoid arthritis and psoriatic arthritis. People who follow this diet eat lots of fresh vegetables and fruits, whole grains, legumes, nuts, olive oil and seeds. They also eat fish, shellfish, white meat and plain fermented dairy, like yogurt and cheese in moderation. They eat red meats, processed meats and sugar only on occasion. This way of eating is also encouraged by Health Canada as part of eating well for health. To learn what Health Canada recommends, check out a sample plate to the left and click here for more information.
Researchers are keen and are doing more work to understand how food affects rheumatic conditions. But this does not change the important message of eating a wholesome and well balanced diet, like the Mediterranean diet, to support health.
video resources
0:00 Opening Remarks – Jennifer Wilson, C+F Executive Director
6:10 Introduction of Speaker, Clinical Dietitian, Inez Martincevic
9:23 The Role of Nutrition and Rheumatic Disease
10:00 Background and Terminology
15:15 Complementary and alternative diets
15:51 The role of diet in rheumatic conditions and symptoms
16:24 Dietary Intervention Study
17:18 Epidemiology
19:18 Diets to treat rheumatic conditions
21:02 Supplements to treat rheumatic disease
27:20 Diet Also matters/ Risk of malnutrition
31:02 The evidence suggests (Diets and Prednisone “Diet”)
32:45 Vegetables, Vegetables, Vegetables
35:39 Whole Grains
37:38 Plant Proteins
39:55 What are Canadians eating?
42:00 Snacks & Snacking
43:21 Healthy Eating Table 1 (Health Canada Recommendations)
44:25 Healthy Eating Table 2 and Healthy Eating Pyramid (Meditteranean Diet)
45:35 Healthy Eating Take 3
45:52 The opposite of healthy eating “The Western Diet”
46:58 Snacks vs. Treats & Snack Ideas
48:55 Strategies for successful healthy eating
50:33 Mindful Eating
51:15 Take out messages from presentation
Audience Q+A
54:50 How do I respond to the many people who believe they can cure my child’s disease with a certain diet?
59:06 My 4 year old was diagnosed with JIA at 18 months. We haven’t been able to get to her iron levels normal. Do ferritin levels increase with inflammation?
1:03:36 Do you have any tips to help get my child to take supplements?
1:07:17 Is dairy considered an inflammatory?
1:09:55 Nightshades. What is the correlation between nightshades and inflammation?
1:12:35 My 8 year old was diagnosed last year. We have cut sugar out in an effort to reduce inflammation. Also, what is your opinion on juicing?
1:17:36. Does gelatin prevent joint pain and discomfort?
1:18:46 If I don’t have access to a dietitian. What resources are available to my family for nutrition?
The Role of Nutrition in Rheumatic Disease
In this session held on February 27th, 2021, Clinical Dietician, Inez Martincevic, of the Hospital for Sick Children will review what we currently understand about nutrition in managing rheumatic diseases including a review of the effects of symptoms and medications on optimal nutritional status, the knowledge and research to date about complementary alternative diets for juvenile arthritis, as well as how to achieve healthy eating for the entire family.
You can access the PowerPoint Presentation here. Plus, Inez answers your questions on snacks vs. treats, ferratin levels and more during the Q+ A session!
Arthritis Broadcast Network: Interview 19 – Cheryl Koehn with Inez Martincevic
Inez Martincevic, a clinical dietician from The Hospital for Sick Children (SickKids) in Toronto, speaks about nutrition and juvenile arthritis.
funding announcement
Cassie + Friends played a pivotal role in helping researchers at SickKids secure a $1,402,240 grant from the Canadian Institutes of Health Research (CIHR) to study the roles of diet and the microbiome on childhood arthritis disease activity – a topic of high priority for families in our community. As part of the study, participants will change their diet for an 8-12 week period and will follow the Mediterranean Diet. Our sincere thanks to all the families in our community who provided their vital feedback to help define and shape this research. This research would not be happening without you. To learn more, visit here and don’t forget to ask about this study in clinic!
nutrition + rheumatic disease f.a.q’s
- Eat 3 meals per day, with snacks in between. Eating regular meals will support your child’s energy levels throughout the day
- Start your day with breakfast. Don’t just have cereal, add some protein. Adding protein to every meal will help your child feel fuller for longer. Examples of protein include eggs, avocado, nut, seed or soy butters, nuts, seeds, hummus, beans, lentils, yogurt, cheese, fish or meat.
- When children are hungry, they often want snacks that are high in carbohydrates such as crackers, bread or toast. Make sure snacks like this also have protein and good fats with them – like nuts, seeds, olive oil, hummus, avocado – which will satisfy them for longer. When choosing carbohydrates aim for whole grains, for example: whole wheat toast with nut butter + piece of fruit, vegetables dipped in nut butter, hummus or guacamole, yogurt with berries and granola
- Oily fish such as salmon, trout, mackerel, sardines and tuna is another great protein. Some fun ways to get kids to eat fish is to try fishcakes or fish tacos.
There are no specific foods that should be eliminated from one’s diet, there are foods however that should be limited.
- Limit sugary foods (cookies, brownies, donuts, sugary cereals), packaged/bottled fruit juices, processed sugary drinks, and snacks. Foods containing high levels of sugar often have little nutritional benefit and may mean your child feels more hungry afterwards.
- Reduce refined foods such as white bread, pasta, and refined cereals – look for whole grain or whole wheat bread, bagels, wraps. Pasta should be whole wheat, or lentil (eg pea or chickpea pasta), cereals should be low in sugar and higher in fiber.
- Limit sodium. Cutting down on salt can lower your risk for high blood pressure, may reduce calcium loss from bones, reducing osteoporosis and fracture risk.
- People with rheumatoid arthritis (RA) may feel the effects of salt even more. Corticosteroids, commonly used to treat RA, cause the body to hold more sodium.
- Limit Saturated fats and Trans fats. Saturated fats are fats that stay solids at room temperature These are found in foods such as meats, butter and cheese. Research has demonstrated that saturated fats have been linked to increased total cholesterol and LDL (bad, cholesterol levels). Trans fat is the process where hydrogen is added to vegetable oil. This process keeps the oil solid at room temperature and extends its shelf life. You’ll find trans fats in commercial baked goods, fried foods and margarine.
someone decides to eliminate gluten, they need to make sure that the child is receiving sufficient
calories, protein, and carbohydrate intakes for adequate growth.
Milk-based products contain all sorts of nutrients and active compounds, including calcium, vitamin D
and a variety of fats and proteins. Choosing lower fat dairy (1% or skim milk) will help to reduce the
saturated fats in milk. Lower fat yogurt and cheese also help reduce saturated fats.Your Content Goes Here
There is no specific evidenced-based research demonstrating that vegetarian or vegan diets are better
in controlling inflammation or JIA. Research has shown that blood levels of vitamin B12, Vitamin D,
calcium and essential fatty acids are lower in individuals following vegetarian, and even lower in those
following vegan diets. If someone chooses to follow a vegetarian or vegan diet, they need to make sure
that the child is receiving sufficient calories, protein, carbohydrates, vitamins minerals and essential fatty
acids for adequate growth.
There is no set amount of protein that should be consumed. However, there should be some protein in
every meal, and ideally in every snack. Examples of good protein sources include; eggs, nuts, seed or
soy butters, hummus, beans, lentils, tofu, lead diary such as low fat milk, yogurt or cheese, fish, and
meat – aim for leaner meats such as chicken or turkey. Beef should be eaten less often (no more than 1-
2 times per week).
There is no specific evidenced-based research demonstrating that turmeric has any positive effects in
controlling inflammation or JIA. There are also no studies done on the safety of consuming large
amounts of turmeric, especially in children. Turmeric can be used as a seasoning for food, but there is
no evidence in using it in large amounts.
may reduce calcium loss from bones, reducing osteoporosis and fracture risk.
People with rheumatoid arthritis (RA) may feel the effects of salt even more. Corticosteroids, commonly
used to treat RA, cause the body to hold more sodium.
Children do not need to be put on low sodium diets, however limiting salt through limiting fast food,
processed foods, snack foods such as chips, salted popcorn, nuts, seeds, pretzels… is recommended.
When cooking to not add excess salt to foods. Try keeping the salt shaker off the table to limit the
addition of extra salt.
C and E supplements may not help, however eating a diet rich in these vitamins is healthy overall.
Foods high in these vitamins = Vitamin D and calcium are important for bone health, supplementing
Vitamin D is only necessary if levels are low, however taking a vitamin D supplement daily is not harmful. Calcium supplements are only necessary if diet is low in calcium. If having 2 servings of low fat dairy per day, then calcium supplementation is not needed
Vitamin and/or mineral supplements beyond what is needed for growth and development (known also as the dietary reference intakes which are based on age and sex) are not needed to boost the immune system in autoimmune conditions. There is little evidence that “more” of a vitamin or mineral, beyond what your teen would get from eating lots of fruits and vegetables, further supports the immune system. Vitamins and minerals are not benign, meaning over-nutrition or over-supplementation can be associated with side effects, so balance is key. Also to note that while red meat is a source of protein it is not needed in the diet. However, a balance of protein sources, such as egg, poultry, fish, pulses, nuts, carbohydrate sources such as vegetables, whole grains and fruits, as well as healthy fats like olive oil, avocado are recommended.
Irish sea moss or seaweed is rich in antioxidants and can be a part of healthy eating. Seaweed has been eaten by many cultures for centuries. However there is no evidence about the safety or efficacy of seaweed in controlling inflammation or treating rheumatic conditions in children. This includes safe doses of seaweed if packaged as supplements. Speak to your healthcare team about seaweed supplements as part of your child’s health.
Fasting and/or intermittent fasting is not advised for either treatment of rheumatic conditions or for weight loss in children and adolescents as this dietary approach may compromise growth and development.
IBD is much like other rheumatic conditions, like JIA or SLE. While there is a lot of interest and research in the area of diet and causes of IBD or dietary causes of flares, there is limited evidence at this time that a diet can treat Crohn’s or UC. There is however very good evidence that one type of diet, called exclusive enteral nutrition, is effective at inducing remission in certain types of Crohn’s disease. Exclusive enteral nutrition is prescribed by a gastroenterologist. Eating well for IBD is very much the same as autoimmune inflammatory rheumatic conditions, with focus on whole real foods, limit packaged/processed foods, rich in whole grains, rich in fruits and vegetables, limiting in red meat incorporating more plant based proteins, and limiting simple sugars/treats.
There is little evidence that food sensitivities/intolerance are associated with disease activity. So food sensitivities/intolerance may not necessarily help with inflammation or pain in arthritis. However some patients do report reduced pain, better mobility and better sleep (thought to be secondary to reduced pain) when avoiding foods that have been identified as sensitivity/intolerance. If you/your child have identified some food sensitivities/intolerances, then speak with your rheumatology team about eliminating these foods from your diet to monitor any effect on inflammation (labs, imaging) and/or pain. CAUTION: multiple food (especially food group) eliminations (for example gluten, dairy, soy, egg and nightshade free diet) can be associated with severe malnutrition, growth faltering, reduced quality of life – so it is strongly advised to eliminate only 2 or 3 foods at a time and seek RD support to ensure that you/your child’s nutritional needs are not compromised.
Gelatin and collagen hydrolysates have been used in pharmaceutical and food products for years, and as such are generally regarded as safe. However the only evidence for potential benefit has been described in adult osteoarthritis, not in pediatric rheumatic conditions. There are also no dosing guidelines for gelatin and collagen hydrolysate supplements in pediatrics. Speak to your Rheumatologist about adding gelatin/collagen hydrolysates as complementary therapy to your child’s current medical regimen, as it may help with pain or discomfort.
helpful links
-
About Kids Health: AboutKidsHealth is a health education website for children, youth and their caregivers from the experts at SickKids Hospital. The website offers a variety of Uveitis and JIA resources for parents and youth.
-
Healthy Eating For Juvenile Arthritis – The Arthritis Foundation: This Arthritis Foundation article discusses food that can promote healthy growth and development in children with arthritis and help dial down inflammation.
-
Popular Diets and Juvenile Arthritis – The Arthritis Foundation: This article breaks down popular diets to explain more about the requirements, evidence and how it relates to children. Learn more about Paleo, Keto, gluten free, vegan and vegetarian diets as they relate to inflammation and juvenile arthritis.