what is JIA?
Juvenile idiopathic arthritis (JIA) is the newest and preferred terminology to describe chronic arthritis in children. The disease is also sometimes referred to as juvenile arthritis (JA) or juvenile rheumatoid arthritis (JRA).
Let’s Break Down the Terminology….
Juvenile – In a young person (usually under 18)
Idiopathic – disease having no known cause or originArthritis – inflammation of a joint
Children under 17 years of age who develop inflammation in a joint (usually with swelling and/or pain and/or morning stiffness) that lasts longer than six weeks usually have JIA. There are seven different types of JIA, and the pattern of arthritis and the short-term and long-term effects of each type are different. We do not know the cause of any of the types of JIA. If the arthritis is associated with another disease such as lupus, dermatomyositis, inflammatory bowel disease or even leukemia, the arthritis is not known as JIA.
hear it from the kids
In Canada, Juvenile Idiopathic Arthritis (JIA) affects 1 in 1,000 kids. That’s over 10,000 kids in Canada alone living with Juvenile Idiopathic Arthritis. Check out the video below to learn more about what JIA is, directly from kids living with it.
quick facts
jia 101 webinar
Hear from parent speaker, Jennifer O’Shea, about her family’s journey with Juvenile idiopathic arthritis, from being diagnosed to pain management and treatments, and from Dr. Roberta Berard, as she shares information on the different subtypes of JIA, the difference between pain and a flare, and emerging research insights. Plus, answers to your questions regarding medications,
• (Lily’s Journey) Q 4:00- How did we know she had arthritis, what were the signs?
• (DR.Bobbi Berard) 14:50-15:25 Q What is Arthritis?
• Q 16:18- What is JIA?
• Q 17:50-Subtypes of JIA.
• 24:21-Kids don’t switch between categories
• 31:41- Treatment
• 34:50- Treatment basses on how many joints and other features.
• 39:40-Individualized medicine in JIA.
• 42:56-Up coming and ongoing studies in Canada.
• 46:00 Q/A
• Q 47:00-What does Lily understand about her condition now and how does she deal?
• Q 48:00- Does she share with her teacher and classmates at school?
• Q 48:55- Difference between pain and flair?
• Q 53:07- Is there a reason why diagnoses are delayed?
• Q 55:36- What doe Biologic mean?
• Q 57:32- Undifferentiated subtype and how it is treated?
• Q 59:00- Can someone have JIA and psoriatic arthritis: can you have two types at once?
• Q 1:01:41- Is there a History of arthritis in family- is there any evidence that it can be passed on?
• Q 1:04:34- Nutrition is there any food categories that increase inflammation?
• Q 1:11:11- What treatments that lily had to overcome?
• Q 1:14:55- Will kids ever grow out of arthritis?
• Q 1:20:28- Any gifts from the journey of arthritis?
additional resources
Arthritis Society and Club Sunrise: The Arthritis Society offers information on Arthritis camp, the Backpack program and additional learning resources such as Taking Charge of your JIA teen program. NEW! The Arthritis Society has added a new virtual event program for children ages 5-17 called Club Sunrise, learn more about it HERE.
About Kids Health: AboutKidsHealth is a health education website for children, youth and their caregivers from the experts at SickKids Hospital. The website offers a variety of Uveitis and JIA resources for parents and youth.
Systemic JIA Foundation: Information and resources specific to Systemic JIA.
f.a.q.’s
Questions answered by the Cassie + Friends Medical Advisory Committee including Pediatric Rheumatologists, Dr. Lori Tucker (BCCH), Dr. Nadia Luca (ACH) and Dr. Roberta Berard (LHSC). You can ask questions anytime and get connected to other affected families by joining our safe and secure Online Support Network! Don’t see your question? Click HERE for even more FAQs!
Children can get chronic arthritis – called juvenile idiopathic arthritis (JIA), previously known as juvenile rheumatoid arthritis – as well as other rheumatic diseases such as systemic lupus erythematosus (known as lupus or SLE), juvenile dermatomyositis, or vasculitis.
About 1 in 1,000 children have juvenile arthritis. This includes children with juvenile idiopathic arthritis (JIA) and those with other rheumatic or connective tissue diseases. If children with orthopedic and congenital problems that may develop into osteoarthritis in adulthood are included, then an average of one to five children in every elementary school have a chronic rheumatic disease.
Juvenile idiopathic arthritis is the newest and preferred terminology to describe chronic arthritis in children. Idiopathic means unknown cause or spontaneous origin. The disease is also sometimes referred to as juvenile arthritis (JA) or juvenile rheumatoid arthritis (JRA). Children under 17 years of age who develop inflammation in a joint (usually with swelling and/or pain and/or morning stiffness) that lasts longer than six weeks usually have JIA. There are seven different types of JIA, and the pattern of arthritis and the short-term and long-term effects of each type are different. We do not know the cause of any of the types of JIA. If the arthritis is associated with another disease such as lupus, dermatomyositis, inflammatory bowel disease or even leukemia, the arthritis is not known as JIA.
JIA is not the same as rheumatoid arthritis! In the United States, some forms of childhood arthritis are still somewhat inaccurately referred to as juvenile rheumatoid arthritis or JRA even though the pattern of arthritis and the short-term and long-term effects of most types of juvenile arthritis are completely different from rheumatoid arthritis in adults. Less than 5% of children with JIA have a subtype of arthritis that resembles rheumatoid arthritis.
A child with arthritis may have an obviously swollen joint, or he/she is stiff when waking up and might walk with a limp, or may have trouble using an arm or leg. Children do not always complain of pain because they may adjust the way they do things so that it hurts less, or they may simply ask to be carried more often. With some of the more serious types of JIA, children may also have a fever, a rash, or feel very weak and fatigued.
Arthritis is diagnosed by examination of the child by a doctor who has specialized training (or experience) in childhood rheumatic diseases. Preliminary evaluation should be by the family doctor or pediatrician, but the final diagnosis is ideally made by a pediatric rheumatologist. There are no blood tests or x-rays to confirm a diagnosis but these tests may be useful to determine the type of arthritis, to assess the severity, or to identify complications.
This is very difficult to predict at the outset, and to some extent, it depends on the type of JIA. In a small number of children, the disease may last as little as several months to a year and disappear forever. Most children, however, have an up-and–down course with “flares” and “remissions” for many years with about half of them continuing to have problems into adulthood. While there is no cure for juvenile arthritis, current available therapy often prevents the long-term damage and disability that may be left by arthritis even after it has gone.
Children with arthritis are not just kids with an adult disease. Although the drugs and therapies used to treat children are similar, the intensity of treatment and the frequency of follow-ups need to be much greater.
Unlike for adults with arthritis for example, physical growth may be stunted, children may grow one leg longer than the other, or one hand or foot may be smaller. Some children with arthritis can also have associated eye inflammation that can lead to blindness. These changes may be irreversible if there is a delay, or poor follow-up, in treatment. The impact of any chronic illness on psychological development, especially during adolescence, should not be underestimated as it can have lifelong recreational, educational, and career implications.
The best outcome for children with any rheumatic disease will be achieved by the involvement of a multidisciplinary team of health professionals such as those at BC Children’s Hospital. In this setting, children will have access to pediatric rheumatologists; specialized nurses, occupational and physical therapists, and social workers whose jobs are dedicated to treatment of children with rheumatic diseases. Other childhood and adolescent medical specialists are also available.
An excellent book is Your Child with Arthritis: A Family Guide for Caregiving by Dr. Lori B. Tucker, Bethany A. DeNardo, Dr. Judith A. Stebulis, and Dr. Jane G. Schaller.
When a child or teen with JIA has active disease, or a flare of disease, in joints in the legs (hips, knees, ankles, feet), it can affect their ability to walk. This is usually due to pain in the affected joints. At the time of JIA diagnosis, approximately 30-40% of children may have some trouble with walking, running, or ability to keep up with their usual activities. Our Canadian research data shows that the majority of children newly diagnosed with JIA can reach inactive disease by 6 months after diagnosis while on treatment- this means their arthritis is controlled on medication. Children with JIA whose disease is controlled on medication are able to walk, run, play sports and keep up with their healthy peers. Overall, in 2020, most pediatric rheumatology teams would see few children with JIA who are needing to use equipment such as crutches or wheelchairs for more than a brief time period.
There are many causes of joint pain in children and adolescents. Arthritis is one we are always on the lookout for. However, there are many other factors that may cause joint pain in children with arthritis and those without. One common example is hypermobility – when the joints are very flexible – which can be associated with some joint discomfort. Other potential causes of joint pain include patellofemoral syndrome (i.e. ‘loose’ knee caps), flat feet, ligament or tendon problems, or overuse. In children with JIA, there may also be some degree of joint damage that could result in persistent pain. There is also some evidence that children and adolescents with JIA can be sensitized to feel more pain because of the prior inflammation. Overall, it is important to bring up pain and other joint symptoms to your rheumatology team so that they can be evaluated and addressed appropriately.
Yes! As a pediatric rheumatology community, we are very hopeful about the effectiveness of our medications and physical rehabilitation as we are successfully able to achieve remission for the majority of our patients. Recent data from research on Canadian children with arthritis has shown that more than 75% of patients will be in remission within 2 years of diagnosis and depending on the subtype this number may be higher. Furthermore, one half of patients are able to stop medications within 5 years of diagnosis. Depending on the subtype, however, some children will have to restart medications within 1-2 years of stopping them because of disease flare. This risk is highest in patients with polyarthritis who have a positive rheumatoid factor; 2/3 of these patients will have to restart medications within the year of stopping. The goal for each patient is to achieve disease remission and thrive in their physical, social and emotional development. For some patients, this will be whilst taking medications long term but for others this may be achieved with medications and maintained after stopping medications. Being able to predict which children will be able to successfully stop medications particularly biologics is an active area of research in our community.
There are 7 recognized subtypes of JIA, and ‘oligoarticular’ disease refers to children who have 4 or fewer joints affected at diagnosis. Some oligoarticular cases can ‘extend’ after 6 months to involve 5 or more joints while others ‘persist’ as oligoarticular. In terms of treatment, this is tailored to the specific patient situation. NSAIDS (naproxen) and cortisone joint injections are often used initially when few joints are affected. However if this is not sufficient for achieving remission, then a disease modifying anti-rheumatic drug (DMARD) — the most common of which is methotrexate – is typically added. The treatment may be the same, whether a child has either oligoarticular or polyarticular disease.
The natural history of arthritis is that it comes in flares, so it is not uncommon to have a flare-up
after remission, especially if you have stopped treatments. Most patients go back into
remission. Sometimes you need to change or adjust your current treatment regimen. If you
stop a medication and get a flare-up, most patients go back into remission after the previous
medication is restarted.
looking for information about other childhood rheumatic diseases?
We have resources pages to help you learn about a variety of diagnoses! Click the links below to learn more.
CRMO Fever Syndromes Vasculitis Juvenile Dermatomyositis Lupus
from our community
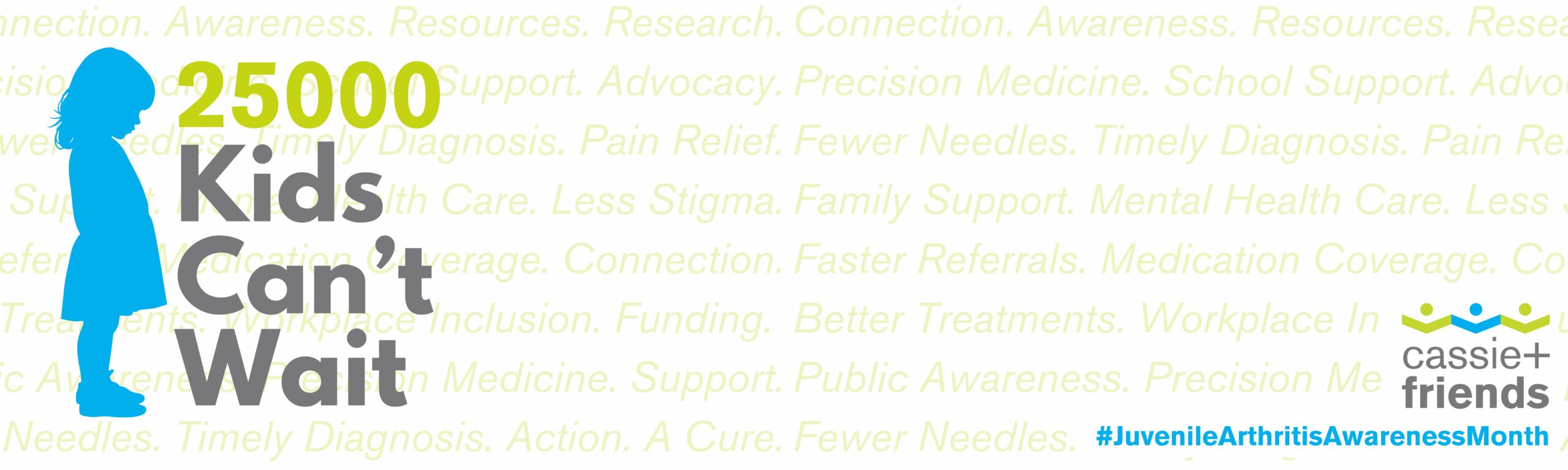
Kids Can’t Wait
Only 1 in 5 Canadians Know Kids Get Arthritis. Help Us Change That. Many people mistakenly believe arthritis only affects older adults but in reality, Juvenile Arthritis is the most common cause of [...]
25,000 Kids Can’t Wait
25,000 Kids Can't Wait. Watch this space for updates on how you can join our campaign to ensure that the 25,000 kids and families affected by JA and other rheumatic diseases have the support they [...]
Where Are They Now: Zahra’s Story
Where Are They Now: Zahra's Story In this special Rare Disease Month edition of “Where Are They Now”, we caught up with Zahra Alidina. In 2023, Zahra shared what life was like living with [...]